Movement Analysis
 |
||
| Contents: | ||
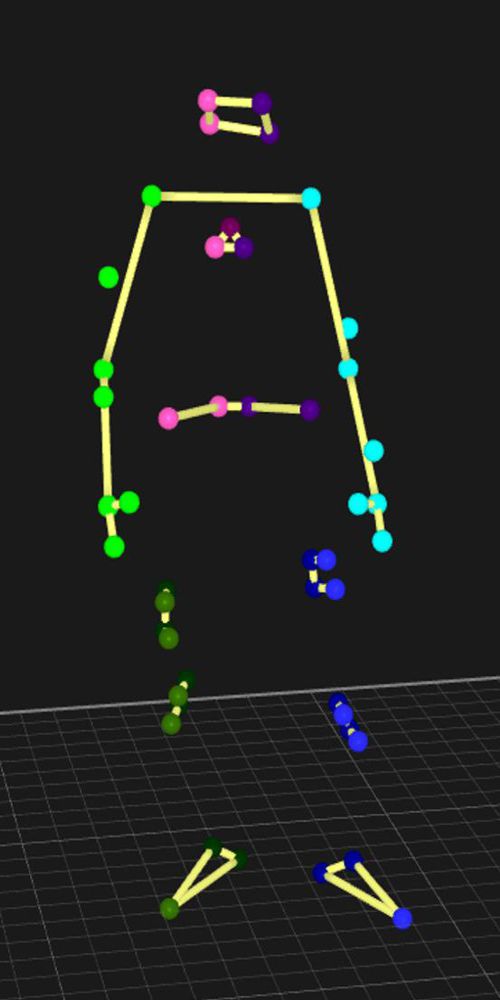
Movements are often analysed by interpretation of the human eye, e.g. medical doctors examining patients. Alternatively, by optical motion capture systems that accurately track the movements of the body, but this requires a complicated setup in a laboratory. This is normally done in a clinical or laboratory setting. However, patients move in a different manner when they know a medical doctor is watching or when their movements are tracked in the lab. Therefore, we want to analyse pathological movement patterns in the natural environment of the patient.
In the last few years, there has been an increasing interest in using wearable sensors, like inertial measurement units (IMUs), to analyse movement patterns. IMUs measure acceleration and angular velocity in 3D. The IMUs can be used to collect data continuously in an unobtrusive and objective manner. The patient only has to wear one or multiple IMUs on the body throughout the day.
IMU data is pretty sensitive to noise, therefore different procedures have to be applied to optimize the signals. Thereafter, the data can be used for example for activity recognition, classification of different diseases or estimation of disease severity. This can help the medical staff to understand and quantify pathological movement patterns of patients. The medical staff can use this information for example to diagnose patients, to monitor disease progression, or to evaluate the effect of treatment.
This research is performed in close cooperation with the Neurogeriatrics group of Prof. Dr. med. Walter Maetzler.
 |
 |
 |
|---|
Corresponding Publications:
R. Romijnders, F. Salis, C. Hansen, ..., G. Schmidt, W. Maetzler on behalf of Mobilise-D Consortium: Ecological Validity of a Deep Learning Algorithm to Detect Gait Events from Real-Life Walking Bouts in Mobility-Limiting Diseases, Frontiers in Neurology, Oct 2023, doi: 10.3389/fneur.2023.1247532
C. Hansen, B. Chebil, J. Cockroft, E. Bianchini, R. Romijnders, W. Maetzler: Changes in Coordination and Its Variability with an Increase in Functional Performance of the Lower Extremities, Biosensors, Jan 2023, doi: 10.3390/bios13020156
S. Paschen, C. Hansen, J. Welzel, J. Albrecht, A. Atrsaei, K. Aminian, K.E. Zeuner, R. Romijnders, E. Warmerdam, P.P. Urban, D. Berg, W. Maetzler: Effect of Lower Limb vs. Abdominal Compression on Mobility in Orthostatic Hypotension: A Single-Blinded, Randomized, Controlled, Cross-Over Pilot Study in Parkinson’s Disease, Journal of Parkinson's Disease, Dec 2022, doi: 10.3233/JPD-223406
R. Romijnders, E. Warmerdam, C. Hansen, G. Schmidt, W. Maetzler: A Deep Learning Approach for Gait Event Detection from a Single Shank-Worn IMU: Validation in Healthy and Neurological Cohorts, Sensors, May 2022, doi: 10.3390/s22103859
C.Hansen, C. Ortlieb, R. Romijnders, E. Warmerdam, J. Welzel, J. Geritz, W. Maetzler: Reliability of IMU-Derived Temporal Gait Parameters in Neurological Diseases, Sensors, March 2022, doi: 10.3390/s22062304
E. Warmerdam, R. Romijnders, C. Hansen, M. Elshehabi, M. Zimmerman, F. Metzger, A.-K. von Thaler, D. Berg, G. Schmidt, W. Maetzler: Arm swing responsiveness to dopaminergic medication in Parkinson’s disease depends on task complexity, npj Parkinson's Disease, October 2021, doi: 10.1038/s41531-021-00235-1
E. Warmerdam, R. Romijnders, J. Geritz, M. Elshehabi, C. Maetzler, J. C. Otto, M. Reimer, K. Stuerner, R. Baron, S. Paschen, T. Beyer, D. Dopcke, T. Eiken, H. Ortmann, F. Peters, F. von der Recke, M. Riesen, G. Rohwedder, A. Schaade, M. Schumacher, A. Sondermann, W. Maetzler, C. Hansen: Proposed Mobility Assessments with Simultaneous Full-Body Inertial Measurement Units and Optical Motion Capture in Healthy Adults and Neurological Patients for Future Validation Studies: Study Protocol, Sensors, August 2021, doi: 10.3390/s21175833
R. Romijnders, E. Warmerdam, C.Hansen, J. Welzel, G. Schmidt, W. Maetzler: Validation of IMU-Based Gait Event Detection During Curved Walking and Turning in Older Adults and Parkinson’s Disease Patients, Journal of NeuroEngineering and Rehabilitation, February 2021, doi: 10.1186/s12984-021-00828-0
A. Pilotto, M. Rizzetti, A. Lombardi, C. Hansen, M. Biggi, G. Verzeroli, A. Martinelli, R. Romijnders, B. Borroni, W. Maetzler, A. Padovani: Cerebellar rTMS in PSP: a Double-Blind Sham-Controlled Study Using Mobile Health Technology, The Cerebellum, February 2021, doi: 10.1007/s12311-021-01239-6
E. Warmerdam, R. Romijnders, J. Welzel, C. Hansen, G. Schmidt, W. Maetzler: Quantification of Arm Swing during Walking in Healthy Adults and Parkinson's Disease Patients: Wearable Sensor-Based Algorithm Development and Validation, Sensors, October 2020, doi: 10.3390/s20205963
R. Romijnders, C. Hansen, G. Schmidt, W. Maetzler: Detection of Walking Bouts from Low Back Accelerometry in a Home-Like Assessment, Biosignale Workshop, 2020, Kiel, Germany
Y. Zhou, R. Romijnders, C. Hansen, J. van Campen, W. Maetzler, T. Hortobagyi, C. Lamoth: The detection of age groups by dynamic gait outcomes using machine learning approaches, Scientific Reports, March 2020, doi: 10.1038/s41598-020-61423-2
E. Warmerdam, R. Romijnders, F. Marin, G. Schmidt, W. Maetzler: Quantification of arm swing during walking, Biosignale Workshop, 2020, Kiel, Germany
E. Warmerdam, J. M. Hausdorff, A. Atrsaei, Y. Zhou, A. Mirelman, K. Aminian, A. J. Espay, C. Hansen, L. J. W. Evers, A. Keller, C. Lamoth, A. Pilotto, L. Rochester, G. Schmidt, B. R. Bloem, W. Maetzler: Long-term Unsupervised Mobility Assessment in Movement Disorders, The Lancet Neurology, February 2020, doi: 10.1016/ S1474-4422(19)30397-7
E. Warmerdam, M. H. Pham, C. Hansen, W. Maetzler: P 130—The Influence of Different Settings on Accuracies of Gait Algorithms, Poster, Gait and Posture, 2018
M. H. Pham, E. Warmerdam, M. Elshehabi, C. Schlenstedt, L. Bergeest, M. Heller, L. Haertner, J. J. Ferreira, D. Berg, G. Schmidt, C. Hansen, W. Maetzler: Validation of a Lower Back “Wearable”-Based Sit-to-Stand and Stand-to-Sit Algorithm for Patients With Parkinson’s Disease and Older Adults in a Home-Like Environment, Front. Neurol., 2018 (doi: 10.3389/fneur.2018.00652)
L. Haertner, M. Elshehabi, L. Zaunbrecher, M. H. Pham, C. Maetzler, J. M. T. van Uem, M. A. Hobert, S. Hucker, S. Nussbaum, D. Berg, I. Liepelt-Scarfone, W. Maetzler: Effect of Fear of Falling on Turning Performance in Parkinson’s Disease in the Lab and at Home, Front. Aging Neurosci., 10:78, 2018 (doi: 10.3389/fnagi.2018.00078)
M. H. Pham, M. Elshehabi, L. Haertner, S. D. Din, K. Srulijes, T. Heger, M. Synofzik, M. A. Hobert, G. S. Faber, C. Hansen, D. Salkovic, J. J. Ferreira, D. Berg, A. Sanchez-Ferro, J. H. van Dieën, C. Becker, L. Rochester, G. Schmidt, and W. Maetzler: Validation of a Step Detection Algorithm during Straight Walking and Turning in Patients with Parkinson’s Disease and Older Adults Using an Inertial Measurement Unit at the Lower Back, Front. Neurol. 8:457, 2017 (doi: 10.3389/fneur.2017.00457)
M. H. Pham, M. Elshehabi, W. Maetzler: Validation of Gait Detection and Analysis, Proc. EMBC, Jeju, Korea, 2017
M. H. Pham, M. Elshehabi, L. Haertner, T. Heger, M. A. Hobert, G. S. Faber, D. Salkovic, J. J. Ferreira, D. Berg, A. Sanchez-Ferro, J. H. van Dieën, W. Maetzler: Algorithm for Turning Detection and Analysis Validated under Home-Like Conditions in Patients with Parkinson’s Disease and Older Adults using a 6 Degree-of-Freedom Inertial Measurement Unit at the Lower Back, Front. Neurol. 8:135, 2017 (doi: 10.3389/fneur.2017.00135)

 We were happy to welcome Sören Lange as a new member of our team at the beginning of the year. In his master’s thesis, he focused on signal processing for innovative underwater opto-acoustic sensor systems and has since then taken on new challenges in the field of magnetic sensors. His research interests span a wide range of topics, including signal processing and control engineering. With his friendly attitude, technical curiosity and expertise, Sören is a great addition to our team. We look forward to working with him!
We were happy to welcome Sören Lange as a new member of our team at the beginning of the year. In his master’s thesis, he focused on signal processing for innovative underwater opto-acoustic sensor systems and has since then taken on new challenges in the field of magnetic sensors. His research interests span a wide range of topics, including signal processing and control engineering. With his friendly attitude, technical curiosity and expertise, Sören is a great addition to our team. We look forward to working with him!